|
|
Posted By Lauren Remspecher,
Wednesday, January 11, 2023
Updated: Wednesday, January 11, 2023
|
We’ve all seen the tragic news stories regarding insulin affordability. A November 2022 report published in the Annals of Internal Medicine estimated that 1.3 million US adults with diabetes (about 16.5% of those diagnosed with the disease) have rationed their insulin use in the past year. This includes those that do not refill their medications on time, skip doses, or take smaller doses – all of which can lead to detrimental health outcomes, and in some cases, even death. But with so much federal attention on the topic and numerous manufacturer assistance programs available to patients, it begs the question: why is insulin affordability still a concern in 2023?
People with Type 1 diabetes do not produce enough insulin to regulate blood sugar levels, but those with Type 2 diabetes develop resistance, becoming less sensitive to the effects of insulin. While people with Type 2 diabetes may be able to function with less-than-ideal levels of insulin, those with Type 1 require a daily dose to survive.
In August 2022, President Joe Biden signed the Inflation Reduction Act into law, which addressed (among many things) the price of insulin. It caps the monthly cost of insulin at $35 for seniors on Medicare. But the law does not address the cost of insulin for the millions of Americans with private insurance. While insulin rationing is more common among low- and middle-income populations and the uninsured, it still occurs among 11% of higher income people and 19% of those with private insurance. Interestingly, rationing was found to be lowest among those with Medicare and Medicaid coverage.
State governments have also taken action, with 20 states now capping copayments on insulin, devices, and diabetes supplies (spoiler alert: Missouri is not one of them). Furthermore, some states, like California, have indicated the intent to start manufacturing their own insulin supply to control costs. As discussed at the 2022 BHC Annual Meeting, a new non-profit funded by a public-private collaboration, called Civica Rx, will also begin selling generic insulin to consumers in the coming year at $30 per vial and $55 for a box of five pens.
Despite federal and state attention to the matter, a 2020 Commonwealth Fund report found dramatic variation in the total cost of insulin, among both the uninsured and those with commercial coverage, with prices ranging from $0 (e.g., a free sample) to more than $1,500 for the same unit prescription. While insulin ingredient costs have remained relatively stable among employers in the BHC’s Pharmacy Management Initiative over the last three years, aggregate plan costs (before rebates) for two insulin products ranked fifth highest among all brand drugs for PMI employers during the 2021 year. What’s more, a 2020 RAND study revealed that insulin prices in the US were five to ten times higher than other countries in the Organization for Economic Co-operation and Development, and still up to four times higher when accounting for potential rebates.
Rebates, distribution costs, and other fees in the pharmacy supply chain have made the issue complicated to address, especially in the commercial marketplace. But for uninsured patients, who may be left paying list prices without a cost-sharing cushion, the impact of insulin pricing is felt significantly. Uninsured patients may also be more likely to use older formulations of insulin, which can make managing blood glucose levels more challenging.
In response to affordability concerns, insulin manufacturers have invested in financial assistance programs for patients. Novo Nordisk, which supplies over 40% of the world’s insulin, offers several affordable options, including:
• Up to three vials or two packs of insulin pens for $99
• Unbranded, therapeutically equivalent biologics at a discounted price
• Free, one-time immediate supply of up to three vials or two pen packs
• Income-based patient assistance programs for free insulin
• Human insulin available at national pharmacies for $25 per vial
• Coupons and copay cards to address high out-of-pocket costs
But not all patients are taking advantage of these offerings. So, what can employers do in 2023 to address insulin affordability concerns? - Educate employees and their family members on lower-priced insulin options that are available.
- Consider the impact of cost-sharing for preventive and maintenance medications on your population, especially lower income workers.
- Monitor insulin adherence with your health plan or PBM and explore clinical programs available to enhance diabetes management.
- Amplify the purchaser voice surrounding medication affordability and monitor regulatory actions on a state and federal level.
In a country where drug prices continue to make headlines, insulin rationing reminds us that this problem is not just about numbers…it’s about lives. And as with many challenges facing our health care system, it will take the collaboration of many stakeholders to find the right solution. In the meantime, the BHC looks forward to supporting our employer members in their benefit, well-being, and advocacy efforts. For other resources to prevent, better manage, and reverse diabetes in your workforce populations, visit the BHC’s Defeat Diabetes Campaign webpage. Warm Regards, Lauren Remspecher, MPH, CHES BHC Senior Director, Member Engagement & Communications
This post has not been tagged.
Permalink
|
|
|
Posted By Todd Boedeker,
Wednesday, December 7, 2022
Updated: Wednesday, December 7, 2022
|
|
The Problem
Despite being pushed off the front pages by the pandemic and our nation’s recent economic woes, deaths from opioid use disorder (OUD) have soared to new levels over the past few years, having a profoundly negative impact on families, communities, and workplaces. According to the
Centers for Disease Control and Prevention, drug overdose is a leading cause of injury-related death in the US, and in Missouri, the leading cause of death for those ages 18-44 years. In 2021, opioids were associated with 70% of all overdoses in the state, at the cost of 1,583
Missouri lives, according to Missouri Department of Health and Senior Services (DHSS) data.
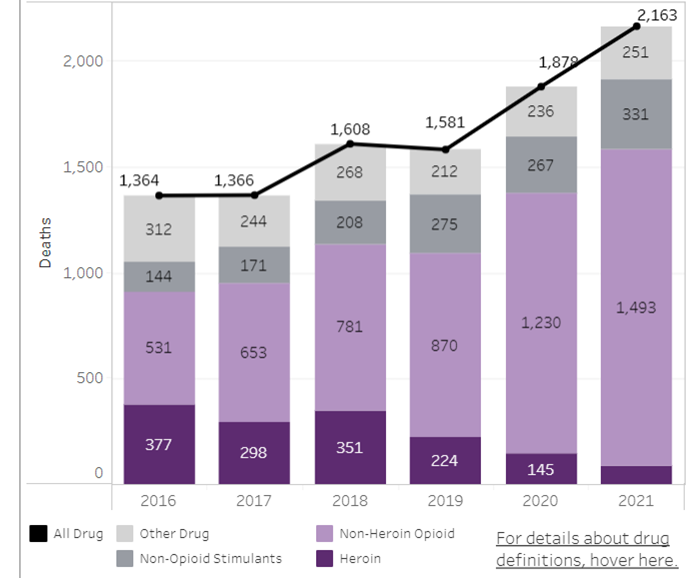
Missouri Resident Overdose Deaths, 2016-2021
Source: Missouri Department of Health and Senior Services
|
|
|
| |
|
|
|
The opioid class of drugs includes heroin, fentanyl, methadone, morphine, oxycodone, and many other prescription and non-prescription pain relievers. As the chart above illustrates, the types of opioids implicated in death from overdose are changing. Synthetic opioids, predominantly illicit fentanyl,
surpassed prescription opioids and heroin
as drivers of overdose-related morality rates in 2016. Much more potent than heroin, fentanyl and its analogues can take the form of powders, tablets, and liquids, which severely challenges efforts to stem opioid misuse.
This enables contamination of a range of illicit drugs, including heroin and counterfeit pills, and has elevated the risk of overdose among low-frequency users and increased both fatal and nonfatal overdose rates.
Reporting from the Midwest Health Initiative demonstrates that opioid scripts per 1,000 in the commercially insured population in St. Louis have been
trending downward, dropping by nearly 25% between 2018 and 2021, likely due to employer, pharmacy benefit manager, and public sector interventions. But this should not be seen as a signal that that all is well at the worksite.
Workplace Impact
According to the Substance Abuse and Mental Health Services Administration, approximately 66% of adults
who misuse opioids are employed. OUD and other substance use disorders increase accidents, turnover, poor job performance, and health care costs. Each employee who recovers from a substance use disorder saves an employer $8,500 annually, according to the National Safety Council (NSC). The
NSC
Substance Use Calculator uses workforce size, industry, and location to calculate the costs of substance abuse for individual businesses.
Employer Action
The drug epidemic affects all genders, races, economic statuses, and age groups in both rural and urban communities.
In addition to workers themselves, any employee may have a partner, child, or family member that is struggling with a substance use disorder. Given the widening scope and continuing urgency of the problem, employers can review and
update their strategies for combatting this serious disease.
- Ensure benefit plans provide supportive counseling and behavioral health services.
- Train managers and workers to identify signs and symptoms of a substance use disorder and connect impacted persons to appropriate treatment and recovery supports.
- Keep naloxone in the workplace and train employees on how to properly administer it. Naloxone reverses the effect of opioids and can save a life, if administered in time. It is available in most states, including Missouri, without a prescription.
- Help employees find the treatment and recovery programs with the highest likelihood of success. Medication
-assisted therapy (MAT) is a comprehensive approach that combines the use of medication with counseling and behavioral therapies to meet the unique needs of individuals.
Missouri DHSS has been working to combat unnecessary death and suffering due to substance abuse, including advancing the number of treatment resources and identifying
MAT Treatment Centers
statewide. For employers in other markets, SAMSHA has a search tool which delivers information on approved treatment programs by zip code. Use care in getting to the actual federal agency site if not using the link provided, as a lot of treatment centers have created “official-looking” sites that promote
their own treatment center.
Resources
Employers hold legal obligations when addressing any type of substance use disorder with an employee. The Americans with Disabilities Act (ADA) protects qualified
employees with disabilities from employment discrimination and may apply to individuals in recovery from substance use disorders. Luckily, there are many resources to guide employers in their efforts, including:
- SAMHSA’s Drug-free Workplace Toolkit,
for advice on complying with federal guidelines.
- SAMHSA’s Guide for Employers to Identify and Prevent Opioid Misuse, a comprehensive and valuable resource for employers seeking effective policies and practices.
- The Society for Human Resource Management has created a library of resources on the topic, including this article on employer treatment approaches to combat rising substance abuse post-pandemic.
- The Minnesota Department of Health’s Opioid Epidemic Response Employer Toolkit,
which includes sample emails, social media, and other resources for communicating with employees about proper disposal of prescription medications and other issues related to opioid misuse.
When employers respond to the opioid epidemic, it benefits employees, the people that surround them, businesses, and society in general. The BHC hosted
an educational program
on this topic in August 2018 and looks forward to continuing to support employers in addressing this concerning public health issue. Please let us know how we can be a resource to your teams.
Warm Regards,
Louise Y. Probst,
BHC Executive Director
|
This post has not been tagged.
Permalink
|
|
|
Posted By Todd Boedeker,
Tuesday, December 6, 2022
|
ST. LOUIS, MISSOURI, December 6, 2022 – The Leapfrog Group announced today that Mercy Hospital Jefferson and Mercy Hospital South have been named to its 2022 national list of Top Hospitals, the only two hospitals in Missouri to be recognized. The elite award is one of the most competitive honors American hospitals can receive in safety and quality. The winning facilities will be officially recognized today as part of Leapfrog’s 2022 Annual Meeting & Awards Dinner.
The St. Louis Area Business Health Coalition is a Leapfrog Regional Leader, working with providers, purchasers, payers, and patients in Missouri to drive safe, high-quality health care.
“We are thrilled to see two Missouri hospitals on Leapfrog’s Top Hospitals list this year,” said Louise Probst, Executive Director, St. Louis Area Business Health Coalition. “Mercy has demonstrated itself to be a leader in safety and quality in our region year-over-year, and we appreciate their partnership in advancing the value of health care for employers, workers, and their family members.”
The Leapfrog Group is a national nonprofit watchdog organization that rates hospitals on how well they protect patients from errors and infections, as well as the effectiveness of procedures and other care they provide. A total of 115 hospitals were selected as Top Hospitals, including: 12 Top Children’s Hospitals, 32 Top General Hospitals, 13 Top Rural Hospitals, and 58 Top Teaching Hospitals.
“It takes a focused effort by every one of our co-workers to earn a Leapfrog A grade,” said Alisyn Beffa, Mercy Jefferson Chief Nursing Officer and Chief Operating Officer. “Going above and beyond that to earn Top Hospital recognition is an extraordinary achievement only a limited number of hospitals can claim. Maintaining the level of care for a second straight year is something our entire community should be proud of.”
The Top Hospital award is given to teaching, general, rural, and children's hospitals that publicly report their performance through the Leapfrog Hospital Survey and meet the high standards defined in the Top Hospitals Methodology. This includes infection rates, maternity care, and a hospital’s ability to prevent medication errors, among other standards.
"Being recognized as a Top Hospital for a second straight year is an honor,” said Dr, Aamina Akhtar, Mercy South Chief Medical Officer. “But the real honor is what this means for our patients and the entire community. They can be assured that when they need us, we will provide the quality, safe care every patient deserves.”
To see the full national list of institutions honored as 2022 Top Hospitals, please visit www.leapfroggroup.org/tophospitals.
About The Leapfrog Group
Founded in 2000 by large employers and other purchasers, The Leapfrog Group is a national non-profit organization driving a movement for giant leaps forward in the quality and safety of American health care. The flagship Leapfrog Hospital Survey and new Leapfrog Ambulatory Surgery Center (ASC) Survey collect and transparently report hospital and ASC performance, empowering purchasers to find the highest-value care and giving consumers the lifesaving information they need to make informed decisions. The Leapfrog Hospital Safety Grade, Leapfrog's other main initiative, assigns letter grades to hospitals based on their record of patient safety, helping consumers protect themselves and their families from errors, injuries, accidents, and infections.
About the St. Louis Area Business Health Coalition The St. Louis Area Business Health Coalition (BHC) is a non-profit organization representing nearly 70 leading employers, which provide health benefits to thousands of lives in Missouri and millions nationally. For 40 years, the BHC has worked to achieve its mission of supporting employer efforts to improve the well-being of their employees and enhance the quality and overall value of their investments in health benefits. To accomplish these aims, the BHC centers its work on providing pertinent research, resources, and educational opportunities to help employers understand best practices for the strategic design (and informed use) of benefits to facilitate high-quality, affordable health care. To learn more, please visit www.stlbhc.org.
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Administration,
Friday, November 18, 2022
Updated: Wednesday, November 16, 2022
|
ST. LOUIS, Missouri, November 18, 2022 – First Busey Corporation (Busey) was announced as the winner of the 2022 Business Health Culture Award at the St. Louis Area Business Health Coalition’s (BHC) 40th Annual Meeting today. With over 1,500 associates nationwide, Busey has established a robust strategy to support holistic well-being, boasting an 89% participation rate among employees.
“It’s more important than ever to take care of ourselves, and Busey’s B Well program provides easy opportunities to do so,” says Van Dukeman, Chairman and CEO of First Busey Corporation. “I’m proud that we prioritize wellness and foster a culture that impacts the health and well-being of our associates and their families."
Empowering associates is core to Busey's mission, vision, and values, and the B Well program is driven by that very passion. Benefits include a 24/7 fitness center, gym reimbursements, online stress management, financial literacy resources, wellness coaches, and a wellness champion network of employees aptly titled “Well-beings.”
“As a BHC member, First Busey Corporation has consistently demonstrated itself as a leader in advancing well-being in the workplace and in our community,” explained Louise Probst, Executive Director of the St. Louis Area Business Health Coalition. “Busey supports their associates in every dimension of wellness, contributing to a healthy organizational culture that helps individuals to thrive."
Created in 2014 by employers of the BHC’s Wellness Roundtable, the Business Health Culture Award recognizes organizations for their innovative and comprehensive approaches to improving the well-being of employees and their family members. The award application was modeled with careful consideration of best practices in the corporate wellness field, as defined by national research organizations, academia, and the employer sector.
To learn more about the award process and resources to support employee and community health, please visit www.stlbhc.org.
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Thursday, November 10, 2022
Updated: Tuesday, November 8, 2022
|
Often not recognized, unbranded generic medications are priced lower in the US, at only 84% of the average paid in comparison countries, according to a Rand study. The average out-of-pocket payment for a generic prescription in a US commercial health plan was just $5.30 in 2021. Today, generics account for 9 of 10 prescriptions filled; yet, only 18% of overall US retail prescription drug expenditures. Brand-name drugs, priced 344% higher in the US, based on 2018 data, are responsible for the significant disparity between drug spending in the US and other nations.
Interestingly, advancing the use of generic medications has been a decades-long cost reduction strategy in the US, ushered in by the Drug Price Competition and Patent Term Restoration Act of 1984. Better known as the Hatch-Waxman Act, unfortunately, this legislation also paved the way for the high-priced brand drug problem the US experiences today. The legislation lengthened the monopolies on brand prescription drugs by up to seven years, despite opposing research that longer patents would substantially increase prescription drug costs to consumers. In an effort to increase the supply of generics and appease the opposition, Hatch-Waxman also enabled manufacturers to make drugs that had gone off patent without having to replicate the same expensive clinical trials. An interesting look back shares the story of how lengthening drug monopolies became the political price for permitting the abbreviated generic drug approval process and the expansion of generic drug use in the US.
Although generic drugs are among the best deals in the US health care system, the generic drug supply has been plagued with problems: dangerous drug shortages, medications tainted with hazardous materials, manufacturers falsifying safety records, and steep price increases for some drugs, including price gouging schemes. It seems that generic prices have become so low that companies have stop making them or cut corners to be able to sustain their business. Few generic drugs are manufactured in the US any longer – making adherence to US quality standards hard to ensure and inspect. According to this New York Times overview of the problem, “competition for market share at rock-bottom price points has led to chronic shortages, unpredictable price-spikes, allegations of illegal price-fixing, and substandard and even dangerous practices.”
According to the article cited above, of the top 100 generic medicines that Americans consume, 83 had no US source of active pharmaceutical ingredients, and no American source existed for 97% of the most commonly prescribed antivirals and 92% of the most commonly prescribed antibiotics. Sudden severe generic drug price spikes, consolidation among drug manufacturers, and access to life-saving drugs for US patients during periods of international unrest have garnered the concern of the federal government, which has been working to shape solutions. An interagency report led by the Food and Drug Administration, entitled Drug Shortages: Root Causes and Potential Solutions, three root causes were identified for drug shortages:
(1) Lack of incentives for manufacturers to produce less profitable drugs;
(2) Market failure to recognize and reward manufacturers for “mature quality systems” that focus on continuous improvement and early detection of supply chain issues; and
(3) Logistical and regulatory challenges that make it difficult for the market to recover from a disruption.
The generic drug supply chain problems demand attention and collaboration from all stakeholders, not just government. Many hospital systems in the private sector have come together to take action, employing a uniquely American solution: competition. The product of their efforts, Civica Rx, now delivers high-quality and fairly priced generic medications produced on US soil. SSM Health is one of the founders of this critical collaboration. Join us at the BHC’s 2022 Annual Meeting where you can learn more about Civica Rx's progress from West Health CEO, Shelley Lyford. Focused on philanthropic efforts to lower health care costs and enable successful aging, West Health will also share the results of their recent research with Gallup focused on American perceptions of health care in the post-COVID era. Warm Regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Thursday, October 6, 2022
Updated: Wednesday, October 5, 2022
|
The St. Louis Area Business Health Coalition’s founders cited the absence of reliable information about the cost differences of health care services as a major driver of their decision to establish the BHC. That was forty years ago, and the lack of this important information has remained a top employer concern throughout BHC’s history. But at last, it seems that the transparency tipping point has arrived, and along with it, new opportunities and responsibilities for employers. In this month's keynotes, we take a look at several of these data sources and the ways that they can be used to drive better value health care.
Advancing price transparency has become a priority on both sides of the congressional aisle, as well as among many public and private organizations. Federal cost reporting requirements for hospitals, health plans, and employers that have been designed and implemented recently all seek to make it easier for patients to price shop. Hospitals must report their actual prices with insurers in a consumer-friendly and machine-readable format. Similar regulations on health plans and employer plan sponsors went into effect this past year, and more are set to come. Although many organizations were slow to comply and the reporting is not standardized, the efforts have provided a national source of hospital prices, ready to be used by patients, employers, and the press to compare care.
Health care claims are the best information source for understanding spending and resource use. They document the care billed by a provider for a patient population. Analyses such as per member per month (PMPM) spending, percent of Medicare facility reimbursement, provider practice patterns and expertise, resource use, and adherence to quality guidelines all hold important insights for driving better value care. BHC's regional partner, the Midwest Health Initiative, engages in these types of commercial claims analyses, as do state all payer claims databases (APCDs).
The National Academy of State Health Policy has undertaken the effort of downloading and organizing data from Medicare cost reports for most US hospitals, including summaries of hospital revenues, expenses, efficiency, breakeven points, charity care, and other financial details. This information is quite useful to employers when comparing hospitals within a community and collaborating with local health systems toward better value care. Thanks to the Centers for Medicare and Medicaid Services, the Leapfrog Group, National Committee for Quality Assurance, and National Quality Forum, hospital-specific findings for a rich set of quality, safety, and patient experience measures are also readily available.
All of this information has the potential to create meaningful competition across medical groups and health systems, driving quality up and prices down. But only if the data get used. Employers are critical to ensuring that our new-found transparency delivers on its promise. Now that we know, or could know, the insights that these data sources hold, we have a greater obligation to act. The BHC is working to organize available data sources nationally and support members in using these insights.
If your organization is ready to take action, here are some steps to get you started: (1) listen to this month’s BHC podcast episode with Mike Thompson of the National Alliance of Healthcare Purchaser Coalitions to be inspired by the possibilities; (2) prepare to talk with your employees about their role in using health care information to be a knowledgeable consumer; (3) join us for the BHC Annual Meeting on November 18th to learn how Americans' perceptions of health care can inform our collective commitment to a better future.
Warm regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, September 7, 2022
Updated: Wednesday, September 7, 2022
|
Last week, Missouri Foundation for Health hosted a forum entitled At What Cost to shine light on the experiences of Missouri patients when using our health system and the resulting cost impact. Dr. Elisabeth Rosenthal, editor of Kaiser Health Network, started the conversation by sharing insights from her book An American Sickness: How Healthcare Became Big Business. She shared 10 points on why American health care is not a market–based system and some of the unfortunate, yet all too common, situations and billing practices that occur and bring financial harm to patients nationally. She gave the example of Duexis, a FDA-approved medication that combines Pepcid and Ibuprofen into one pill, and is known to most employers as a prime example of a low-value pharmaceutical. When purchased over the counter, this therapy would cost about $11 per month, but when written by a physician as a single prescription, the cost is over $2,300 a month. Dr. Rosenthal asks the important question, "Why do we allow this?" She noted that no other nation would.
She also cautions patients, that when being told that you may need to spend a night in the hospital, to confirm that your services will be classified as an inpatient stay and not an observation visit. Although the room and level of care is the same, an observation visit is considered outpatient care and will likely be subject to much higher patient cost sharing than an inpatient stay.
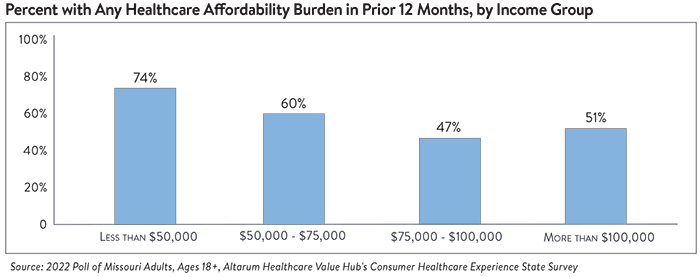
Altarum, a nonprofit research organization, fielded its Consumer Healthcare Experience State Survey to more than 1,100 Missouri adults during April 2022. The survey results unmask Missourians’ perceptions on a wide range of health system issues, including prescription drug costs and health care affordability. A few of the key findings include: - 62% of respondents experienced at least one health care affordability burden in the past year, including 51% of respondents with family incomes more than $100,000.
- 82% worry about affording health care in the future;
- 60% of uninsured adults under the age of 65 say they have postponed getting the health care they needed due to cost, as did about half (48%) of insured adults.
- Lower-income respondents and respondents with disabilities reported higher rates of going without care and incurring debt due to health care costs.
- Adults ages 25-34 years rationed medication due to cost more often than any other age group.
More than two-thirds of respondents believe Missouri’s health care system needs to change. Respondents, across party lines, express strong support for government-led solutions. They cited drug companies, hospitals, and insurance companies as the main drivers of out-of-control costs and identified a number of ways the government could tackle these issues. Sheldon Weisgrau, Missouri Foundation for Health’s Vice President of Health Policy stated, “This is not a partisan issue. Missourians want policymakers working together on solutions that will make a real difference in their lives and ensure people get the care they need at a price they can afford.” Curious about survey results in other states where you may have employees? Check out Altarum’s Healthcare Value Hub.
The good news is that many provider, health plan, labor union, and employer leaders agree. In fact, over the summer they have been meeting to discuss shared opportunities to improve health care affordability and quality. To learn more about the American public’s perceptions of health care and efforts to reduce the growth in health care spending, we invite you to attend our 2022 Annual Meeting on Friday, November 18, in St. Louis, Missouri. Tickets are complimentary for BHC members, and travel stipends are available to assist out-of-town members in attending. We look forward to sharing our progress with you and celebrating our 40th anniversary as employer partners in health care. Warm regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, August 10, 2022
Updated: Tuesday, August 9, 2022
|
Among the innovative technologies that could boost health outcomes and value, Digital Therapeutics (DTx) hold great promise. A June 2022 National Academy of Medicine report suggests that DTx could yield earlier diagnoses and treatments; more effective, coordinated, and continuous care; stronger patient engagement; and greater efficiency – all through a convenient smartphone app or video game.
So what exactly are Digital Therapeutics?
According to the non-profit trade association, Digital Therapeutics Alliance, DTx deliver medical interventions directly to patients using evidence-based, clinically evaluated software to treat, manage, and prevent a broad spectrum of diseases and disorders. DTx services are distinct from the many health and wellness apps that simply track calories or count steps in that they are specifically designed to treat disease. Early DTx have focused on asthma, anxiety, diabetes, post-traumatic stress disorder, and ADHD, with solutions for a wider range of conditions under development. DTx may use sensors and AI-based algorithms to provide real-time feedback to patients and providers or offer customized coaching. What are Prescription Digital Therapeutics?
Prescription Digital Therapeutics (PDT) are subject to peer-review clinical trials that confirm their ability to improve peoples' lives. They receive FDA approval and are prescribed by a clinician. PDT can be used in conjunction with other medications or therapies, or as standalone treatments under a clinician’s oversight. A few leading, FDA-approved PDT include: - Pear Therapeutics has three prescription software treatments for substance use disorders and insomnia.
- Akili’s EndeavorRx prescription videogame treatment helps children with ADHD improve attention function by navigating a space ship through obstacles.
- EaseVRx, by Applied VR, is a virtual reality software that uses cognitive behavioral therapy to reduce lower back pain with relaxation techniques, distraction, and behavior modification.
- BlueStar, developed by Welldoc, is prescribed for adults with Type 1 or Type 2 diabetes to suggest in real-time when users should test their blood sugar and how to control it by adjusting food intake and exercise.
What should be considered when evaluating DTx? DTx advocates think most disease conditions will include a software solution as a first-line therapy in the next decade. Yet, payers and providers have been slow to embrace these technologies. Eager to create pathways for reimbursement, product innovators have pursued distribution through the major Pharmacy Benefit Managers, some of which now offer PDT formularies. Early-adopter employers are beginning their due diligence in evaluating available PDT with the following questions: (1) Clinical and Cost-Effectiveness - Is the evidence strong enough to pay for treatments that resemble free or low-cost smartphone apps? How will cost-effectiveness be measured and reported? What is the expected duration of treatment and cost? Given their newness, a standard FDA process for vetting PDT does not exist. As the controversy surrounding Biogen's Alzheimer's drug made clear, employers cannot always use FDA approval as a proxy for clinical effectiveness. Fortunately, PDT innovators are hustling to amass an evidence base for their products. Employers should expect evidence of clinical trials and value to exist, along with indicators of patient acceptance. Kaia Health, for example, points to a randomized controlled trial showing that patients using its solution to treat lower back pain had medical claim costs that were 80% lower than those using standard therapy. Performance guarantee should be expected. Bipartisan legislation in the pipeline may expand Medicare coverage of PDT. If this passes, the coverage of specific products by the Centers for Medicare and Medicaid Services could be a helpful indicator of clinical and cost-effectiveness. (2) Purchasing Intermediary and Process - A digital “formulary” is a catalogue of vetted apps that PBMs or health plans offer. Would your organization prefer to go through one of these intermediaries to purchase or go direct? Do PDT have rebates and administrative fees, and are these disclosed? Does your health plan or PBM contract ensure that all revenues earned from products or services used by your enrollees are returned to the plan sponsor? (3) Patient Cost and Plan Design - Does your plan design language need to be updated to account for PDT and DTx? How will patient cost sharing being structured and the benefit of PDT be communicated? Ready to explore further? While DTx and PDT could be attractive solutions for patients, physicians, plans, and employers, many questions remain to be answered. BHC members looking to learn more are invited to attend our next Pharmacy Meeting on September 13 at 2:00 PM (CT) as we discuss the PDT and DTx landscape, offerings currently available through PBMs, and considerations for employers prior to implementation. Warm regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Todd Boedeker,
Thursday, July 7, 2022
Updated: Tuesday, July 12, 2022
|
An important new mental health resource goes live this month: a three-digit national hotline for all mental health crises, including suicide and substance abuse. Federal legislation passed in July 2020 requires all phone carriers to transfer “988” calls to the National Suicide Prevention hotline, which will connect the individual to a network of local mental health professionals ready to respond in every state. While available nationally, the federal legislation left funding for the local response network to each state, many of which have yet to do so. Fortunately for those of us in Missouri, Governor Parson and our legislature have funded the program, at least initially, and the Missouri Department of Mental Health (DMH) has met the challenge of organizing our state's response. While intended to work like the national 911 hotline for emergencies needing police, fire, or medical care responders, there is one important distinction. The new 988 hotline is not directly linked to law enforcement; rather, it connects callers with crisis-trained mental health counselors and other appropriate resources. This practice is in keeping with the National Association of Mental Illness' campaign “Help Not Handcuffs,” so as to avoid unnecessarily escalating mental health crises and putting law enforcement officers into situations that that they may not be best equipped to handle. Under DMH’s guidance, six regional hotline centers have been designated, connected, and trained to be able to quickly support Missouri callers. Individuals can call, chat, or text 988. “The goal of 988 is to change the way our community responds to mental health crises,” said Debra Walker, spokeswoman for DMH. “It will serve as the first line of defense to engage individuals experiencing mental health or suicidal crisis. With a strong, well-funded crisis system in place, Missouri will have the ability to divert mental health crises away from costly, already burdened resources, including our criminal justice and health care resources.” DMH expects Missouri will see a reduction in ER visits, inpatient stays, arrests, and incarceration related to mental health and substance use disorders. According to the DMH website, the intervention may include assessment, stabilization, referral, and follow-up for individuals at high risk for suicide and/or poor mental health outcomes. If a higher level of care is needed, the crisis specialist will work with the caller and other supports to connect them to a mobile crisis response team in the community. You can learn more about Missouri’s 988 hotline here. Suicide is a leading cause of death and a critical public health problem in the United States. It was responsible for 46,000 deaths in 2020 alone. According to CDC statistics, an estimated 12.2 million American adults seriously thought about suicide that year, 3.2 million planned a suicide attempt, and 1.2 million attempted suicide. More positively, 90% of those that attempt suicide and survive go on with their lives and never die from suicide. While many factors contribute to suicide, it can be prevented, and everyone has a role to play. You can help by spreading the word about the new 988 hotline, knowing the warning signs of suicide, and supporting social changes which reduce the stigma associated with behavioral health conditions and build personal resilience and coping and problem-solving skills for individuals and communities. Warm regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, June 8, 2022
Updated: Wednesday, June 8, 2022
|
An estimated 37 million, or 1 in 7 adults, in the United States have Chronic Kidney Disease (CKD). Unfortunately, 90% don’t know they have the condition until it’s too late to prevent its serious and expensive consequences. It doesn’t have to be like this. In an impressive display of collaboration and an unprecedented timeframe for change in health care, the National Kidney Foundation (NKF), National Committee for Quality Assurance, and other national organizations have aligned their levers to build important groundwork to improve the diagnosis and prognosis for people with or at risk of chronic kidney disease. NKF is now turning to physicians, health plans, employers, and patients to pick up the cause. Read on to learn about the diagnosis and treatment of kidney disease, connect with resources, and understand how you can take actions to protect your workforce and the people important to you from chronic kidney disease. The kidneys are vital to life. They remove excess toxins from the blood, balance key electrolytes and fluid volume, and excrete hormones that help regulate blood pressure, red blood cell production, activate vitamin D, and support bone strength. The primary cause of kidney disease is diabetes, followed by hypertension. CKD increases the risks of heart disease, stroke, and early death, in addition to kidney failure. Many people with CKD die of a heart attack because of the strain that kidney failure places on their heart. Practice guidelines now recommend two screenings, a blood and a urine test, annually to assess for kidney disease among people with diabetes, hypertension, or other risk factors for CKD. The blood test is the estimated glomerular filtration rate (eGFR) and it assesses kidney function. The urine Albumin-to-Creatinine Ratio (uACR) assesses kidney damage. Both are needed. In 2020, major laboratories collaborated to create a standardized kidney profile that bundles the eGFR and uARC into one request, which more easily enables clinicians to order and compare results across labs. It’s not a urine dipstick. Convenient and commonly used in the physician office to check for protein in the urine, dipstick urine tests do not detect lower albumin and creatinine levels and are not recommended for assessing kidney damage. Often the earliest sign of CKD, an elevated uACR (≥30 mg/day) can detect kidney damage about 10 years before a decline in eGFR is observed, so at-risk patients should get an uACR. To improve treatment outcomes, race is no longer included in the eGFR equation. African Americans and Hispanics are disproportionately affected by CKD and are more likely to progress to kidney failure than Whites. However, it has been recognized that race is a social and not biological construct, including race when assessing screening results could unintentionally worsen disparities in care. This led to a taskforce recommendation that the adjustment for race be removed. African American and Hispanic patients may find changes in their kidney disease status or stage when they are first tested by a lab which has completed this transition.
A single quality measure now includes both tests. The Kidney Health Evaluation for Patients with Diabetes was developed by the National Kidney Foundation and the National Committee for Quality Assurance (NCQA) for implementation in 2021, and public reporting of results is expected in 2022. The Centers for Medicare & Medicaid Services has also begun to transition a similar measure into its Merit-based Incentive Payment Systems (MIPS) programs. Due to recent debate around the numerical definition of hypertension, NCQA was unable to include people with hypertension in the measure denominator at this time. Screening rates in people with hypertension need further attention.
Screening rates are way too low. The average testing rate for people with diabetes is less than 50% nationally, which leaves an enormous number of people in the dark about their disease. Kidney screening rates in Missouri lag the nation. With support from Bayer, the Midwest Health Initiative (MHI) was able to apply the new NCQA measure to statewide data, learning that in 2021 only 40.9% of commercially insured adult Missourians with a diagnosis of diabetes received these two kidney tests. Congratulations to Esse Health for a top screening rate of 67.8% in the St. Louis region. The US Preventive Services Task Force announced last month that due to new evidence and treatments that support assessing asymptomatic patients, it would re-evaluate adding screening for chronic kidney disease (CKD) to its list of preventive services. Employers have an important role to play in advancing screening. Early diagnosis and treatment can meaningfully reduce suffering, save lives, and lower spending. Ask your health plan to provide a baseline screening rate for your at-risk population. Align your health education and wellness strategies with those of your vendors to increase screening rates. Talk with your physician, friends, and family about kidney screening. These changes have occurred recently and rapidly. Not all providers are aware of them, so it’s important for patients at risk to request the tests.
Education and resources from the CDC, NKF, and a toolkit from NCQA and Bayer are also available. The BHC stands ready to support your efforts. Please reach out with any questions or requests. Warm Regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|