|
|
Posted By Louise Probst,
Thursday, May 5, 2022
Updated: Wednesday, May 4, 2022
|
With nearly 20% of the US economy now consumed by health care expenditures, it is important to consider how this level of spending impacts the public. Thanks to the foresight and collaboration of two organizations, West Health and Gallup, results from a large and comprehensive survey on the state of health care in America provide important insights. Fielded during the pandemic, the survey reveals the opinions of more than 6,600 adults in all 50 states. Spoiler alert: it isn’t pretty.
Here are a few of the highlights: - Negative perceptions of the US health care system related to cost, quality, and access grew dramatically over the course of the COVID-19 pandemic. Nearly half of all Americans surveyed (48%) say their view of the US health care system worsened due to the pandemic.
- An estimated 38 million Americans (15%) report that their ability to pay for health care has become worse due to the pandemic, resulting in a greater portion of Americans delaying and deferring needed care.
- Few Americans believe they receive good value when weighing the quality of care against the cost. An overwhelming majority of Americans (93%) agree citizens across the country are paying too much for the quality of care received. This view is consistent across all income groups and has increased significantly throughout the year.
- More than a third (35%) of respondents say they are “more worried” about affording health care in the future, a concern shared by at least one in five households making more than $90,000 a year. One-fifth of Americans (21%) report a time in the prior 12 months when they or a household member had a health problem worsen after postponing care, with Medicaid beneficiaries (37%) reaching nearly the same level as the uninsured (39%). Black adults are twice as likely as White adults to know someone who died because cost kept health care out of reach.
- When falling ill, 73% of Americans report being somewhat or very worried about insurance covering the cost of treatment. Among respondents, there is more concern about the cost of care than missing work or finding a provider to treat the illness. For many Americans, the cost of care may worsen their health conditions due to both care avoidance and added anxiety.
- More than two-thirds of Americans, regardless of party affiliation, say they are pessimistic about the federal government enacting policies to reduce health care costs in the coming year. Two-thirds of US adults (66%) think voters have very little to no power in reducing the cost of health care in the US, but nearly nine in 10 think American businesses, corporations, and US Congress do.
The report points out that this overwhelmingly negative public sentiment has been years in the making. Tim Lash, President of West Health, sums the report up like this: “Bottom line – Americans are increasingly getting priced out of the system, and many of those who can still afford to pay don’t think they’re getting their money’s worth relative to the cost. We must begin to change this trajectory with smarter policies that put patients over profits.” So what happens next? Will politicians in Washington and across state governments feel the public's pain and finally take meaningful action to lower costs, improve access, and reduce inequities? The BHC will continue advocating on behalf of purchasers, businesses, and workers that they do. Warm Regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Thursday, April 7, 2022
Updated: Wednesday, April 6, 2022
|
On behalf of patients, purchasers, and the public, the Leapfrog Group is a leading voice for safer, higher quality, and more transparent health care. The impetus for its formation was the Institute for Medicine’s urgent call to action and report, To Err is Human. Published in the American Journal of Medicine in 1999, it made it perfectly and publicly clear: medical mistakes are a top cause of preventable harm and death in the United States.
Leapfrog's advocacy started with a simple three-question survey of hospitals. If implemented, each recommendation represented a potential giant leap forward for patient safety. So straightforward and obviously important from today’s lens, it’s hard to understand the pushback that was initially received, with hospitals discrediting the “science” and boycotting the survey. Leapfrog knew all too well that what is was asking was expensive and that the technology was not perfect. Yet, it also understood that the technology would not get better until it was used and that the cost of not acting was both expensive and harmful.
Leapfrog's first three leaps are still included in its annual, voluntary hospital questionnaire. With results available publicly online, patients, purchasers, and providers can all ask if their hospital has:
(1) Computerized Physician Order Entry (CPOE)
With federal financial support, more than 95% of hospitals have implemented Electronic Health Records (EHRs). Few would consider going back to the old ways of handwritten orders. One report suggests that medical errors have decreased 52% as a result of online ordering, and three times as many physicians reported that their EHR prevented a potential medication error rather than cause one. Yet, there is more to be done. A November 2021 report finds that 7,000 to 9,000 Americans die due to a medication error each year. The total cost of looking after patients with medication-associated errors exceeds $40 billion each year, with over seven million patients affected.
(2) ICUs staffed with intensivist physicians during daytime hours (can be partially met with telemedicine)
The benefit of having patients cared for by physicians trained in critical care has been well-researched and found to reduce ICU mortality and spending. A recent study published in the Journal of Thoracic and Cardiovascular Surgery found that 24-hour intensivist coverage was associated with lower mortality, lower rates of cardiac arrest, and shorter durations of mechanical ventilation. Interestingly, the practice of a trained intensivist physician assuming responsibility for ICU patients' care has been the mainstay in Europe for decades. According to a 2016 report, only about half of hospitals in the US meet this criteria, and practices vary widely by state.
(3) Enough surgical volume to safely perform certain high-risk procedures
Unknowingly, patients are often at greater risk of death and complications because their surgical teams do too few procedures (even common ones) for doctors, nurses, and technicians to maintain their skills. For 10 high-risk surgeries, Leapfrog asks hospitals to report their case volumes annually. In 2015, knowing that patients in the hands of low-volume surgeons or hospitals tend to fare worse, a group of leading academic institutions asked all hospitals to “Take the Volume Pledge” to improve surgical outcomes. Johns Hopkins, a leader in this initiative, explains the importance of surgical volume to its potential patients and lists the frequency of 11 procedures performed at its hospitals on its website.
The evidence that volume matters to surgical outcomes is strong. This 2015 US News and World Report article discusses the issue from a variety of perspectives and provides examples of the importance of volume for surgical cases, including for common surgeries such as a knee replacement.
The takeaway: a low volume surgeon or hospital may provide a good outcome, but overall patients are likely to have fewer complications and better outcomes in the hands of an experienced surgeon and facility. While it would be nice, we do not have to wait for hospitals to take the volume pledge. Don’t be shy about asking a surgeon directly, or the physician that refers you to a surgeon, for the number of times that they completed this surgery at the recommended facility in the past year.
Leapfrog was founded to shine a light on hospital performance so that employers and patients could use their purchasing power to reward the top achievers and foster a marketplace for high-value care. Leapfrog reporting has expanded. Today you will find a letter safety grade for every general hospital in the US, as well as measures of infection rates, Cesarean section rates, and health equity.
Leapfrog’s success depends on all of us using information to seek the safest and best quality care. The BHC is proud to support this effort as a Leapfrog Regional Leader in the St. Louis area. We will continue to highlight Leapfrog advancements and support employer members and the public in accessing and understanding the information. Please let us know how we can assist as you explore the available data. Warm Regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Administration,
Friday, March 25, 2022
|
In a new Missouri Times editorial, BHC Executive Director, Louise Probst, addresses how HB 1677 and SB 921 could increase health care costs for Missouri businesses and families. Click here to read the full article.
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, March 9, 2022
Updated: Wednesday, March 9, 2022
|
A recent headline grabbed my attention: the National Institute for Health and Care Excellence (NICE) recommends the United Kingdom’s National Health Service (NHS) cover the new weight loss medication, Wegovy. Given that England’s NHS review process was characterized as a “death panel” by some in the US not long ago, I was eager to understand the details of this recommendation. Both countries recognize obesity as a top driver of poor health and high health care spending and report that more than 60% of their populations are either overweight or obese.
By way of background, Wegovy is a once a week injectable semaglutide, a medication that mimics the GLP-1 hormone (glucagon-like peptide-1). Released after eating, GLP-1 suppresses appetite and slows gastric motility, making people feel full longer and eat less. Clinical trial data show that participants lost on average 12% more of their body weight compared to a placebo over a 68-week period. Weight loss was found to be higher when combined with a supervised weight loss program. Studies have shown that weight returns, though, when the medication is stopped, suggesting this would be a lifelong treatment. Since its June 2021 US Food and Drug Administration (FDA) approval, Novo has experienced supply chain issues which have limited the drug's availability and postponed its marketing efforts to physicians. Supply chain issues are expected to be resolved in the coming months. Early indications suggest that patient success and physician acceptance is favorable and that product awareness and use are beginning to pick up.
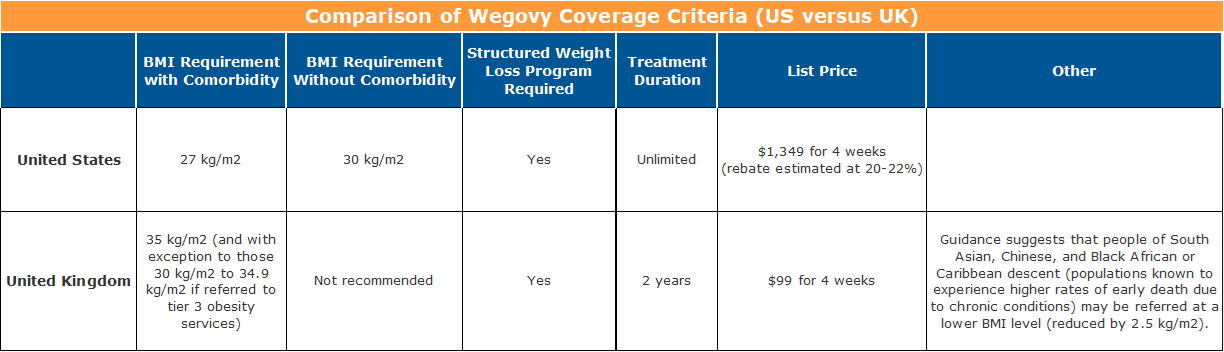
The FDA approved Wegovy for use, in addition to a reduced calorie diet and increased physical activity, for patients with at least one weight-related ailment and a body mass index (BMI) of 27 kg/m2 or greater, as well as for people with or without an obesity comorbidity at a BMI of 30 kg/m2 or greater. Weight-related conditions include high blood pressure, type 2 diabetes, or high cholesterol.
NICE’s independent appraisal committee recommended that Wegovy be considered as an option for weight management when offered alongside a supervised weight-loss program for a maximum of two years. Patients must have at least one weight-related condition and a BMI of 35 kg/m2 or greater. With exception, patients with a BMI of 30.0 kg/m2 to 34.9 kg/m2 may be considered if they meet certain additional criteria. Individuals from a South Asian, Chinese, and Black African or Caribbean background (known to experience higher rates of preventable premature death) were recommended for consideration at a lower BMI (usually reduced by 2.5 kg/m2).
But what about the price differences?
Novo has set the list price for Wegovy in the US at $1,349 for a four-week supply. Rebates are generally understood to be about 20% to 22% of the list price. This means that net of rebates, Wegovy will cost over $13,000 per patient per year in the US.
In the UK, not so much. Wegovy has a list price of about $99.08 (£73.25) for a four-week supply, or just under $1,300 per patient per year. So before any negotiations off of the list price, the annual cost in the UK is less than a one-month, after-rebate supply in the US.
We all know that the US has a very different and cumbersome supply chain, especially when compared to a single-payer system like that in the UK. So I was prepared for a price that was double, triple, or maybe quadruple – but not ten times or more.
Why is it priced so much higher in the US? Well, it seems that it is the usual answer…“because it can." Wegovy is but one example of a problem we see often in the US pharmaceutical industry.
The Institute for Clinical and Economic Review (ICER), the US' non-profit, private-sector response to the UK’s NICE, has announced that it will undertake a review of Wegovy this fall. Using an open, transparent, and independent consensus-based process, ICER reviews medications and establishes a fair price for use in the US. ICER leaders have been giving a lot of thought to how employers in the US could leverage this work to achieve better value for their investments in pharmaceuticals. Several possible solutions in their forthcoming Purchaser Playbook hold appeal. BHC members can get a sneak peek at these recommendations, and we look forward to receiving your feedback. Let’s not despair. Let’s take action.
Warm Regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, February 2, 2022
|
Overseen by the Department of Labor, the Employment Retirement Income Security Act (ERISA) clearly defines fiduciary standards required of the individuals that make decisions related to employer-sponsored health benefit plans. They must: - Act solely in the interests of plan participants and beneficiaries;
- Carry out their duties prudently;
- Follow the plan documents (unless inconsistent with ERISA);
- Hold plan assets (if the plan has any) in trust; and
- Pay only reasonable plan expenses.
Every ERISA plan must have at least one person identified and accountable for having decision-making power over the health plan’s fiduciary actions. The duty to act prudently, a central theme of ERISA oversight, focuses on the diligence exercised in the processes and evaluations leading to fiduciary decisions. It requires expertise in a variety of areas and the ability to seek the best value on behalf of plan participants. Accepting this responsibility, employers invest heavily in the education and training of their internal team and also enlist the expert guidance of an array of benefit consultants, actuaries, and clinicians. When selecting an administrative partner, such as a PBM, a number of vendors are thoroughly evaluated, extensive financial modeling occurs, and prices and contract terms aggressively negotiated. Benefit managers, HR professionals, executive leaders, and Boards of Directors fully appreciate the seriousness of their fiduciary responsibilities in administering a health benefit plan under ERISA and the potential liability that exists if they are found not to act in the best interest of plan enrollees. Some organizations name an administrative committee or their Board of Directors as their fiduciary, and most require the final approval of fiduciary benefit decisions to be reviewed and approved at the highest levels of the organization before enacted. So it is incredibly frustrating when legislative bodies bring forth bills that directly interfere with an employer's fiduciary responsibility to its plan participants. Yet, this is exactly what Missouri House Bill 1677 does. It places the financial interest of independent pharmacists over the financial interest of Missouri workers, their families, and the state’s employers. It disregards the commitment and effort undertaken by ERISA plan sponsors to act solely in the interest of plan participants and carry out their duties prudently. It is also hard to see how the legislature can enact legislation which would increase health benefit costs for workers, without some fiduciary responsibility. At the direction of the BHC Board and on behalf of members, small businesses, and all Missouri workers, the BHC has submitted a letter to the Health and Mental Health Policy Committee of the Missouri House of Representatives opposing House Bill 1677. The letter outlines BHC’s concern in three areas that we feel threaten to reduce pharmaceutical competition, increase costs, and constrain plan management strategies. We will continue to follow this and other legislation, some that more directly targets employers’ ability to overcome the significant mark-up on specialty medications administered in the medical benefit. We welcome your input and engagement after you review the legislation and BHC’s letter. Please reach out to share your thoughts and support. We recognize the difficult challenges faced by brick and mortar retailers and empathize with the small independent pharmacies. These are difficult times for most businesses and many families. But it is not the time to pass legislation which favors one business model over another, especially when consumer behavior trends clearly demonstrate a continued and accelerated preference for online and home delivery services. It is not the time to take programs demonstrated to be effective in reducing cost off the table. Warm Regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Todd Boedeker,
Wednesday, January 26, 2022
Updated: Tuesday, April 5, 2022
|

|

|
| |
|
|
ST. LOUIS, Missouri, January 26, 2022 – The St. Louis Area Business Health Coalition (BHC), the region’s only organization focused solely on representing the purchaser perspective on health care, is celebrating its 40th year. Founded in 1982 by a small group of leading employers, the coalition now serves nearly 70 member organizations across the U.S. that provide health benefits to thousands of lives in Missouri and millions nationally. In collaboration with local health system, health plan, and other community partners, the BHC has worked to advance its mission of supporting employer efforts to improve workforce well-being and the value of health benefit investments.
The coalition’s history and success would not be possible without the guidance of its Board of Directors, comprised of experienced human resources and benefits professionals from the region’s top businesses. The New Year kicked off with the announcement of new Executive Committee leadership, as the BHC welcomes 2022-2023 Board President,
Dave Toben, Director of Benefits, for Bi-State Development/Metro Transit.
"The BHC has played an important role in advancing health care in our region for decades, and I am honored to serve as Board President during such a momentous time in the organization's history," said Dave Toben. "As we embark on our 40th year, I am eager to continue strong collaborations with fellow employer purchasers, seeking higher quality and more affordable health benefits for our employees and their family members."
Other Executive Committee leaders include Vice President
John Ziegler (Arch Resources), Treasurer Marla Langenhorst
(Ameren Corporation), and Member-at-Large Bryan Kassing (Concordia Plan Services). The BHC also looks forward to insights from four new Board members, inducted for their first three-year terms:
|
|
Linda Brady
Healthcare Strategy & Policy
The Boeing Company
Valerie Peters
Vice President, Human Resources
Olin Corporation
|
Margo Quinlan
VP, Total Rewards/Payroll HCM
Schnuck Markets, Inc.
Chad Thompson
Corporate General Manager of HR
North American Lighting, Inc.
|
|
In addition to serving its employer members with education/networking events, group-purchased benefit offerings, well-being programming, and data benchmarking tools, the BHC will focus on several priority projects during the 2022 year. These include multi-stakeholder partnerships to improve overall health and the value of health care across our region. The BHC and its Board are also engaged in health policy and legislative discussions on a state and national level, ensuring that the interests of those buying and using employer-sponsored health coverage are represented.
To stay informed of these efforts or to view a full list of BHC’s Board of Directors and membership, please visit www.stlbhc.org. Community partners are also encouraged to follow the BHC on Twitter and LinkedIn to join in this year’s anniversary celebration using the hashtag #BHCturns40.
|
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, January 5, 2022
Updated: Wednesday, January 5, 2022
|
Blood transfusions save millions of lives in the United States every year. They help patients survive traumatic injuries, undergo surgery safely, or minimize the impact of cancer. They save the lives of new mothers threatened with massive obstetric hemorrhage and sustain the lives of premature babies. A 2020 report to Congress notes that transfusions are one of the most frequently performed procedures in U.S. hospitals, being used by more than 5% of all patients. But today, there is a severe shortage in our nation’s blood supply. Donor turnout, which has declined over the past decade, has now also been dramatically impacted by the pandemic. Blood centers across the country are reporting less than a one-day’s supply of blood — a call to action for all of us. Dr. Rhonda Cooke, Chief of Pathology at St. Louis’ Missouri Baptist Hospital, has reached out to solicit businesses’ help to spread the word about the dangerously low blood supply and to encourage employees to prioritize blood donation in Missouri, nationally, and around the world. “I have never seen blood shortages as severe as what we are currently experiencing. If the nation’s blood supply does not stabilize soon, life-saving blood may not be available for some patients when needed,” says Dr. Cooke, who has practiced transfusion medicine for more than 10 years. The American Red Cross (ARC) informed hospitals in December that they will not be able to fill orders for Group O blood for at least the next 4 to 6 weeks. Physicians have been notified that a triage process is in place and that some patients may need to delay surgeries and will likely not have access to transfusions. Blood use has dropped by about a third in the past decade, largely because of improvements in surgical technique and blood conservation efforts, according to Kaiser Health News. But this has not been enough to offset the declines in donation, as many regular donors age. For people who grew up during World War II — and their children, the Baby Boomers — blood donation was a civic duty that became a lifelong habit, said James AuBuchon, President and Chief Executive of Bloodworks Northwest in Seattle. Nearly 60% of blood donations come from people over 40 according to the AABB, an international non-profit focused on transfusion medicine and cellular therapies. Increasingly, blood industry experts report that there are too few young people lining up to replace them. Our nation’s blood supply is almost entirely dependent on volunteer donors and the network of 66 federally regulated non-profit blood centers. While only 37 percent of the U.S. population is eligible to donate blood, less than 10 percent do annually. Donors must be at least 18 years old (16- and 17-year-olds must have written parental consent). There is no upper age limit. COVID vaccination does not prevent or defer donation, as long as you are healthy and symptom-free. Typically, the blood comes from an anonymous person. However, people may donate blood to directly benefit a friend or loved one, and in some cases, themselves. Given the shortages, this may be something to consider. What can YOU do? First, if you can, please donate. Giving blood is a charitable act, and like other charitable acts, it strengthens values and helps the donor feel good. Organizing incentives or steps to make it easier for or to reward your employees who make this donation can be beneficial for their health and well-being. Here are some other recommended actions: - Help prioritize blood donation as a national imperative by increasing public awareness and education around blood donation, especially for younger and diverse donors.
- Reach out to BHC for sample articles and periodic reminders to inform your workers and encourage their donation throughout the year. Be sure to include information about donation centers and eligibility criteria. For more details, visit the websites of the ARC, AABB, or ABC.
- Inform your employees of organized opportunities that may spur their donation. This month, the American Red Cross is raffling off Super Bowl tickets to those that donate. The St. Louis Cardinals host an annual blood drive among their fans, and the 2022 BIG Heart Blood Battle was recently launched across four Big Ten schools: Michigan, Michigan State, Penn State, and Wisconsin.
- Consider sponsoring a competitive challenge across the divisions of your organization or with a supplier or another employer. If you go this route, BHC is here to assist you in finding resources to support your planning and execution.
Thank you for your actions to sustain America’s blood supply. Warm regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, December 8, 2021
Updated: Wednesday, December 8, 2021
|
The 2021 No Surprises Act provisions to protect the public from the most painful of surprise bills, air ambulance transport, will take effect January 1, 2022. Yet, the controversy over establishing a process to identify a “fair” payment rate remains under dispute.
Congress directed federal agencies, including the U.S. Department of Health and Human Services (HHS), to establish a federal Independent Dispute Resolution (IDR) system to be available for use after thirty days of unsuccessful negotiations between a payer and air ambulance provider. Under the proposed IDR system, an approved arbitrator entity would receive information about each party’s claim, additional requested information, and the “qualified payment amount” (QPA) or the plan’s median in-network payment. Modeled after the “baseball-style” arbitration, the IDR entity selects one offer, which becomes binding on both parties. The losing party must pay the fees associated with the IDR process.
Recognizing that billed charges can be inflationary and that public program rates are significantly lower than commercial payments, Congress barred the IDR arbitrators from considering: (1) a provider or facility’s usual and customary charge or the billed charge; or (2) reimbursement rates paid by public payers. The law lists the QPA as a must-be considered factor and gives the IDR the authority to determine how other factors influence their determination. These other “additional factors” likely include geography, market share, service expertise or level, etc. The IDR entity is also required to explain their decisions when selecting an offer that is higher than the QPA.
Both the Association of Air Medical Services (AAMS) and the Texas Hospital Association have filed suits in federal court challenging the proposed rules. According to a December 6th Health Affairs blog post, both suits claim that the agencies have given priority to the QPA, and as such, the new federal IDR process favors insurers. The lawsuits claim that the rules are not consistent with what Congress intended because of the heavy weight placed on the qualifying payment amount in the arbitration process.
Administration officials, purchasers, plans, and patients believe that the agencies did what Congress instructed. Their goal was for the IDR process to help to lower health care spending, and they find that many of the provisions are necessary to encourage the parties to work together in earnest to resolve their dispute, rather than relying the arbitration process. If QPA is not considered, they fear that patients, employers, and public insurance programs could face higher premiums.
Hotly debated and lobbied political issues are a strong indication of the amount of money on the table. Operating as an “out-of-network” provider has brought price-setting power to air ambulance companies and hefty profits. Research from the USC-Brookings Schaeffer Initiative for Health Policy revealed that by 2017, two private equity firms controlled nearly two-thirds of the national Medicare market for both fixed-wing and helicopter air ambulance transports and that transports delivered by private equity and publicly-traded firms were the most expensive, often reimbursed at 50 percent more.
According to Heathcare Dive, Congress is also weighing in on the rules, with 152 lawmakers signing a letter on November 5 stating the latest rules "do not reflect the way the law was written, do not reflect a policy that could have passed Congress…” Besides stating the obvious, since these issues were debated for months in Congress, before the details were assigned to the federal agencies to determine, their letter seems to value the financial interest of the private equity firms above that of the American public. The Healthcare Dive article links you to the letter and 152 Congressional signors. Take a look and see what you think.
Stay tuned. Resolution of these pending lawsuits is expected in early 2022. Warm regards, Louise Y. Probst BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Administration,
Thursday, November 18, 2021
Updated: Wednesday, November 17, 2021
|
ST. LOUIS, Missouri, November 18, 2021 – Special School District of St. Louis County (SSD) was announced as the winner of the 2021 Business Health Culture Award at the St. Louis Area Business Health Coalition’s (BHC) 39th Annual Meeting today. With staff in over 265 public schools across 22 districts in St. Louis, SSD becomes one of only eight employers to be recognized with the annual distinction.
The mission of the SSD Employee Wellness Program is to improve the health and well-being of employees and promote healthy lifestyles which, in turn, fosters an environment to enhance student success.
“Wellness has always been an important issue,” says SSD’s Superintendent of Schools Dr. Elizabeth Keenan, “but the COVID-19 pandemic has required us to review and revise how we meet the increased health care needs of our staff.”
As the COVID-19 pandemic unfolded and employees adapted to a new way of teaching and working, benefit leaders at SSD quickly pivoted their well-being strategy. Supported by a Worksite Wellness Mini-Grant from the Missouri Department of Health and Senior Services, SSD expanded virtual exercise class offerings through the Wellbeats platform and created fitness rooms at two buildings. Four LC500 Health Kiosks were also purchased to allow employees and school visitors to check their weight, blood pressure, and body mass index (BMI) onsite.
“As a BHC member and local employer, Special School District of St. Louis County has consistently demonstrated itself as a leader in advancing well-being in the workplace and in our community,” explains Louise Probst, Executive Director of the St. Louis Area Business Health Coalition. “SSD has successfully created a culture of health for its staff and families by embedding wellness into its organizational mission and strategic goals. Even amidst a global pandemic, SSD continued to support the physical, mental, emotional, financial, and social factors that impact employee health and happiness on a daily basis.”
Created in 2014 by employers of the BHC’s Wellness Roundtable, the Business Health Culture Award recognizes organizations for their innovative and comprehensive approaches to improving the well-being of employees and their family members. The award application was modeled with careful consideration of best practices in the corporate wellness field, as defined by national research organizations, academia, and the employer sector.
To learn more about the award process and resources to support employee and community health, please visit www.stlbhc.org. ###
About the St. Louis Area Business Health Coalition
The St. Louis Area Business Health Coalition (BHC) is a nonprofit organization representing over 70 leading employers, which provide health benefits to thousands of lives locally and millions nationally. For 39 years, the BHC has worked to achieve its mission of supporting employer efforts to improve the well-being of their employees and enhance the quality and overall value of their investments in health benefits. To accomplish these aims, the BHC centers its work on providing pertinent research, resources, and educational opportunities to help employers understand best practices for the strategic design (and informed use) of benefits to facilitate high-quality, affordable health care. To learn more, please visit www.stlbhc.org or follow the BHC on Twitter and LinkedIn.
This post has not been tagged.
Permalink
|
|
|
Posted By Administration,
Wednesday, November 10, 2021
Updated: Wednesday, November 10, 2021
|
St. Louis, Missouri, November 10, 2021 – The Leapfrog Group, a non-profit representing hundreds of the nation’s most influential employers and purchasers of health care, and supported by the St. Louis Area Business Health Coalition (BHC) as a regional leader in Missouri, announced today the
fall 2021 Leapfrog Hospital Safety Grades.
The independent grading system assigns an “A,” “B,” “C,” “D,” or “F” grade to general hospitals across the country based on over thirty national measures of preventable errors, injuries, accidents, and infections. The fall 2021 Hospital Safety Grade represents the largest set of hospitals ever graded, with grades assigned to 2,901 facilities across the country.
In the St. Louis and surrounding region, twenty-six (26) hospitals were graded, and ten (10) earned an “A,” five (5) earned a “B,” eight (8) earned a “C,” one (1) earned a "D," one (1) earned an “F,” and one (1) was not graded.
The local hospitals that earned an “A” include HSHS St. Elizabeth's Hospital, Mercy Hospital Jefferson, Mercy Hospital South, Mercy Hospital St. Louis, Mercy Hospital Washington, OSF Saint Anthony's Health Center, SSM Health St. Clare Hospital – Fenton, SSM
Health St. Joseph Hospital – Lake St. Louis, St. Luke’s Des Peres Hospital, and St. Luke’s Hospital.
The Leapfrog Hospital Safety Grade is the only hospital ratings program based exclusively on hospital prevention of medical errors and harms to patients. The grading system is peer-reviewed, fully transparent and free to the public. Grades are updated twice annually, in the fall and spring.
“The Leapfrog Group thanks the health care workers in St. Louis and nationwide who work so hard for their communities. It’s important we recognize excellence, especially in times like these. But it’s also important to know when hospitals fall short, because lives are at stake,” said Leah Binder, president and CEO of The Leapfrog Group. “We see every day how hospitals can and will improve their safety when patients make clear it’s important to them.”
For more information about the Leapfrog Hospital Safety Grade, as well as individual hospital grades and state rankings, please visit HospitalSafetyGrade.org.
About The Leapfrog Group
Founded in 2000 by large employers and other purchasers, The Leapfrog Group
is a national non-profit organization driving a movement for giant leaps forward in the quality and safety of American health care. The flagship Leapfrog Hospital Survey and new Leapfrog Ambulatory Surgery Center (ASC) Survey collect and transparently report hospital and ASC performance, empowering purchasers to find the highest-value care and giving consumers the lifesaving information they need to make informed
decisions. The Leapfrog Hospital Safety Grade,
Leapfrog's other main initiative, assigns letter grades to hospitals based on their record of patient safety, helping consumers protect themselves and their families from errors, injuries, accidents, and infections.
About the St. Louis Area Business Health Coalition
The St. Louis Area Business Health Coalition (BHC) is a non-profit organization representing over 70 leading employers, which provide health benefits to thousands of lives in Missouri and millions nationally. For 39 years, the BHC has worked to achieve its mission of supporting employer efforts to improve the well-being of their employees and enhance the quality and overall value of their investments in health benefits. To accomplish these aims, the BHC centers its work on providing pertinent research, resources, and educational opportunities to help employers understand best practices for the strategic design (and informed use) of benefits to facilitate high-quality, affordable health care. To learn more, please visit www.stlbhc.org
or follow the BHC on Twitter
and LinkedIn.
This post has not been tagged.
Permalink
|
|