|
|
Posted By Louise Probst,
Wednesday, February 3, 2021
Updated: Wednesday, February 3, 2021
|
President Biden pledged that fighting COVID-19 and protecting the U.S. from another pandemic would be his top health care and economic priority. Although it has only been two weeks in office, his intentions are taking shape. In the first 24 hours, the United States reversed its prior decision to leave the World Health Organization (WHO) effective July 2021 and rejoined its consortium to share coronavirus vaccines fairly around the globe. Honored, Dr. Fauci announced this decision to a virtual and cheering audience of the world’s public health leaders. He shared that the U.S. will work with them to strengthen and transform WHO, transparently investigate the organization’s initial response to the pandemic, and prevent the next outbreak from becoming a pandemic. A COVID-19 Taskforce of experienced public health and infectious disease leaders was established, as was the COVID-19 Response Office, responsible for coordinating the pandemic response across all federal departments and agencies. The new National COVID-19 Coordinator will report directly to President Biden. Day two, Biden released a 200-page document, National Strategy for the COVID-19 Response and Pandemic Preparedness. While those that have been following the national dialogue on pandemic response will not find much new, it is an organized plan with clearly stated goals, with a commitment to follow science-based interventions, be transparent, and coordinate actions.
Importantly, it recognizes testing as a critical public health tool in tracking and fighting this and future pandemics and commits to expanding testing supplies. The federal government’s role in ensuring the production and supply of adequate protective equipment is defined. An Executive Order directs the Occupational Safety and Health Administration (OSHA) to create standards to ensure the safe reopening of schools, businesses, and travel. Most businesses and schools have already taken many of the steps to protect their workers and customers, as outlined in OSHA’s Protecting Workers: Guidance on Mitigating and Preventing the Spread of COVID-19 in the Workplace. Yet, employers will want to monitor these as they may be expanded and become requirements, rather than recommendations. The Biden administration aspires to fixing more than COVID-19 when it comes to health care. Expanding coverage through increased federal subsidies, particularly among those residing in states that have yet to expand Medicaid, is included in Biden’s stimulus plan, and a recent Executive Order reopened and made changes to support broader enrollment in the Affordable Care Act (ACA) marketplaces. While these needed actions make access to care more affordable and equitable for low-income families, they do little to reduce health care spending. Prominent in Biden’s campaign claims were furthering transparency, bringing accountability to drug pricing, and the more controversial additions of a public option and reducing the eligibility age for Medicare. There is only so much that can be done by Executive Order. Steps needed to reduce health care inflation to levels at or below overall economic growth will require legislative action and be more difficult to achieve, even with the recent Democratic wins in both chambers of Congress. While off to a good start, it’s too soon to tell if the bipartisan support needed to finally transform American health care into the high-value system we all want and deserve has arrived. Warm Regards, Louise Y. Probst, BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, January 6, 2021
Updated: Wednesday, January 6, 2021
|
2021 has arrived, and along with it has come several sunny winter days and a slightly flatter COVID-19 case curve than our region experienced a month ago. While we all need to remain vigilant about social distancing and other public health measures, there are reasons for optimism. In particular, the long-awaited and heavily debated federal actions outlined below, which position our health system to deliver better health care value to patients and communities. They hold promise for the future.
Most Surprise Medical Bills Soon to be Stopped
After years of failed legislative efforts, Congress acted late December to protect patients from most surprise bills. Beginning January 1, 2022, patients will no longer be able to be charged more than they would have paid for an in-network service in two types of scenarios: (1) when they find themselves in an out-of-network facility or air ambulance in an emergency situation, or (2) when they use the service of an out-of-network provider while seeking care in an in-network facility. Ground ambulances, the most common type of surprise bills, were left out. This was due to congressional leaders’ inability to understand the impact on the diverse types of ambulance companies, particularly those serving small municipalities. In an effort to stop these as well, a commission to study surprise bills for ground ambulances was established. The law now requires the out-of-network provider and insurance company to arbitrate and set guidance for the factors to be considered by the independent arbitrator in establishing a fair price.
Hospital Transparency is Expanded
Widely contested price transparency measures went into effect January 1, 2021, after the courts fail to be swayed by the American Hospital Associations’ claims of unfair burden and upheld the Trump administration’s rules for price transparency. Facilities must post the following information on their website for each service and product: (1) charges, (2) negotiated rates with insurance company, noting the lowest and highest negotiated price, without disclosing which insurer received which rate, (3) self-pay price offered to patients without coverage or paying their own claim, and (4) the bundled price for 300 common “shoppable” procedures or services, 70 of which have been defined in the rule by HHS. These are to be posted online, in a machine-reasonable and consumer-friendly format. A quick look at several local hospital websites did not find them to be fully compliant. Yet, there are signs that they are moving to become more transparent. Similar regulations, effective January 2022, have been imposed on insurers.
Payment Alignment Lays Foundation for Stronger Primary Care
CMS has prevailed in making changes to the CPT coding system and payment rules designed to streamline provider documentation and realign payments to better reward physicians for their time spent in evaluation and management of patients, as compared to the time spent doing procedures. It went into effect January 1. Devised to be budget neutral, the expected $9.9 billion in higher payments has been offset by decreases in the conversion factors for some services. The AMA estimates the impact to provider practices will range between a decrease of 10 percent and an increase of 16 percent. This is a long-awaited and important step in advancing primary care in the U.S. health system. More details can be found
here
.
Moving into the New Year, the BHC will continue to monitor legislative activities on a local, state, and federal level that have an impact on health care quality, affordability, and safety, as well as employer-sponsored benefit plans. We welcome the opportunity to connect with your organization’s policy leaders to discuss priorities and shared action that can be taken in 2021.
Warm Regards,
Louise Y. Probst,
BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Annie Turner,
Tuesday, December 8, 2020
Updated: Wednesday, December 9, 2020
|
ST. LOUIS, Missouri, December 8, 2020 – Concordia Plans was announced as the winner of the 2020 Business Health Culture Award at the St. Louis Area Business Health Coalition’s (BHC) 38th Annual Member Business Meeting today. Serving a national workforce of over 28,000 employees at more than 6,000 ministries, Concordia Plans becomes one of only seven employers to be recognized with the annual distinction, including past winners Parkway School District and Anheuser-Busch Companies, LLC.
“At Concordia Plans our vision is healthy and engaged workers serving in thriving ministries,” said James Sanft, President and CEO of Concordia Plan Services of The Lutheran Church–Missouri Synod. “Our team does a fantastic job of supporting those workers through their life events and stepped up in 2020 to serve a membership that faced unprecedented challenges. We are dedicated to providing resources that care for the health and well-being of our own team and their families and that can positively impact the way they serve and all aspects of their lives. We are very thankful for this great honor.”
Created in 2014 by employers of the BHC’s Wellness Roundtable, the Business Health Culture Award recognizes organizations for their innovative and comprehensive approaches to improving the well-being of employees and their family members. The award application was modeled with careful consideration of best practices in the corporate wellness field, as defined by national research organizations, academia, and the employer sector.
“As a BHC member and local employer, Concordia Plans has consistently demonstrated itself as a leader in advancing well-being in the workplace and in our community,” explained Louise Probst, Executive Director of the St. Louis Area Business Health Coalition. “Concordia Plans has successfully created a culture of health for its workers and families by embedding wellness into its organizational mission and strategic goals. In 2020, Concordia Plans quickly adapted to the challenges as a result of the COVID-19 pandemic to continue supporting the physical, mental, emotional, financial, and social factors that impact employee health and happiness on a daily basis.”
To learn more about the award process and resources to support employee and community health, please visit www.stlbhc.org/page/WorkplaceWell-being.
###
About the St. Louis Area Business Health Coalition
The St. Louis Area Business Health Coalition (BHC) is a nonprofit organization representing over 70 leading employers, which provide health benefits to thousands of lives locally and millions nationally. For 38 years, the BHC has worked to achieve its mission of supporting employer efforts to improve the well-being of their employees and enhance the quality and overall value of their investments in health benefits. To accomplish these aims, the BHC centers its work on providing pertinent research, resources, and educational opportunities to help employers understand best practices for the strategic design (and informed use) of benefits to facilitate high-quality, affordable health care. To learn more, please visit www.stlbhc.org or follow the BHC on Twitter and LinkedIn.
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, December 2, 2020
Updated: Tuesday, December 1, 2020
|
As COVID-19 ravages, the news that a vaccine is just around the corner offers a bright light on a potentially dark winter. Pfizer, BioNtech, and Moderna’s vaccines have reported high efficacy rates in clinical trials. The FDA is scheduled to vote
on
Emergency Use Authorization
for Pfizer’s vaccine on December 10, with the first doses already traveling by plane to centralized positions. Limited
quantities of vaccine are expected by the end of 2020, with supplies increasing substantially in 2021.
Aside from the administrative logistics, hurdles remain in the form of awareness and misinformation. All of us have a role to play in dispelling myths and getting out the facts. Here are five things everyone should know about the COVID-19 vaccine:
(1) Is it normal to feel sick after getting vaccinated? When people feel bad after a vaccine, they often claim they got sick from the vaccine or had a bad reaction. Vaccines work by giving the body a preview of
the virus so that the immune system can recognize it and develop antibodies to fight it. Chills, fever, and muscle aches are common following a vaccine and a sign that it is working.
(2) Does the shortened approval process for a COVID-19 vaccine compromise safety? The FDA is expediting vaccine availability through Emergency Use Authorization (EUA). EUA is used in a public health emergency when the benefits of a product that hasn’t received full FDA approval outweigh any risks. It is important to emphasize
that all COVID-19 vaccines are rigorously tested on tens of thousands of people in multi-phase clinical trials that are overseen by established safety control boards and protocols. Additionally, the CDC follows long-established protocols to ensure
the
safety
of COVID-19 vaccines.
(3) When can I get a vaccine? Following CDC guidance, the state of Missouri has created a
COVID-19 Vaccination Plan
laying out a phased rollout to priority populations. Early doses will target frontline health care workers and long-term care facility staff. The focus then moves to critical infrastructure workers, those ages 65 and up, and communities at higher
risk of severe COVID-19 outcomes. Supplies are expected to expand substantially in 2021. It is anticipated that 90 to 180 days after initiation the vaccine will become broadly available to any adult who wants one.
(4) Who will pay for the vaccine? The federal government is using taxpayer dollars to distribute the vaccine and ancillary personal protective equipment (PPE) to providers at no cost. Anyone who wants and needs
a vaccine can get one free of charge. Providers may charge a fee to cover the cost of administering the vaccine and seek reimbursement from private and public health insurers.
(5) How many doses are needed? The first vaccines likely will require
TWO doses. This is standard for many FDA-approved vaccines. The second shot boosts a vaccine’s effectiveness, especially for older people. Unfortunately, this brings a potential drop-off rate after the first dose. Educating employees and the public about
this upfront will reduce this occurrence.
COVID-19 vaccine administration plans are being updated regularly. The BHC is tracking the CDC and Missouri plans – stay tuned for more information as it become available.
Warm Regards,
Louise Y. Probst,
BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Thursday, November 19, 2020
Updated: Thursday, December 3, 2020
|
Despite promising
news on vaccines, the pandemic continues its grip on Missouri and the St. Louis
region. Our state reported 6,346 new COVID-19 cases on Saturday, the most by
far since the pandemic began in March. The COVID-created health and economic
challenges are likely to persist for months to come, experts say. The only thing
that remains unknown is how we as a region and a state will react to it.
Last week, the St.
Louis Metropolitan Pandemic Task Force and the Missouri Hospital Association
separately called on state officials to provide greater leadership on pandemic
issues, including support for a statewide mask mandate and creation of
“safer-at-home” programs to slow or stop the spread of infection.
Hospital admissions
have typically followed spikes in new cases by about two weeks, doctors across
the country have reported. As hospitals in the St. Louis region already grapple
with “unsustainable” levels of COVID-19 cases, doctors worry that the worst is
yet to come. “At that point, we would not have the capacity we need to
sufficiently care for our patients. Not just COVID patients, but all patients,”
said Dr. Alex Garza, an emergency medicine physician and chairman of the
pandemic task force.
Gov. Mike Parson has
repeatedly said that while he does not support a statewide mask mandate, “It is
imperative that Missourians take personal responsibility and social distance,
wear a mask, practice personal hygiene and limit their gatherings.”
Some may see
tradeoffs: supporting our economy or taking on the virus. But that’s a false
dichotomy. Both issues must be addressed together. Only then will the economy
be able to resume growing and the health and well-being of Missourians be best
supported.
The St. Louis Area
Business Health Coalition (BHC) commends the work of the Pandemic Taskforce and
hospital leaders and our local elected officials as they mobilize to stop the
spread of the virus. Like others, BHC would like to put these problems in our past. To do this, we must slow the spread of infection now, to avoid overwhelming hospitals and health care providers during the weeks
to come.
Aligned leadership
from state and regional officials is important, but it is absolutely crucial
that citizens lead the way. The ask of us is really simple: Mask up, wash your
hands frequently, take care of your health, and limit social gatherings to
those in your personal bubble.
In St. Louis County,
new restrictions went into effect on November 17. But parts of Missouri with
the highest rates of new infections are currently rural, sparely populated
counties where no mask mandates are in place and where basic infection control
practices are rarely publicly practiced. Counties with the highest rates of
new cases as of Monday morning were Gentry, Perry, and Moniteau, where case
rates are about double that of St. Louis County. Jefferson and St. Charles
counties also had higher rates than St. Louis County.
Heading into winter,
the stakes are high for everyone in our region and across our state. We
recognize that small businesses and restaurants are hurting. But allowing the
virus to continue spreading unchecked will only prolong the pain and, in a very
literal sense, the suffering of those who become infected.
We should all be
doing what we can to support those small businesses, and to thank the thousands
of health care workers in our communities who have put their personal lives on
hold to battle against the virus on the front lines.
Most of all, we have
to work together defeat this virus. The choice is in everyone’s hands.
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Thursday, November 5, 2020
Updated: Tuesday, November 3, 2020
|
Congratulations, we made it! Election Day is here, at last. With 100 million of Americans reported to have voted before Tuesday, November 3, and large early morning crowds in socially distanced lines at the polling places, the U.S. is expected to reach record highs for voter turnout, despite pandemic concerns. Many thanks to the state and local public officials and employees, and the army of volunteers that made casting our votes in this election both safe and convenient, including the newly available drive-by voting for people infected with COVID-19, which I happened to see this morning. The large number of cars lined up and volunteers in protective gear was a pleasant reminder of American’s shared commitment to democracy, and also, a sad reminder of COVID-19’s reach. Again, health care registers as a top issue among voters. ACA rules that expand access to coverage and remove barriers to those with pre-existing conditions are valued by most people. Estimates find that 135 million Americans had some preexisting condition pre-pandemic; that number is likely to have grown as a result of COVID-19’s lingering symptoms. Fortunately, both presidential candidates have vowed to keep the ACA provisions which enable this. Gaining insight into the federal health policy agenda post-election will require additional days, weeks, and months. The outcome of the Supreme Court’s deliberation of California vs. Texas, a case challenging the ACA’s constitutionality, is expected mid-2021. As an expansive piece of legislation, the ACA has enough provisions for most people to find things that they deeply appreciate and others that they strongly oppose. The list is long. What I find most often underappreciated about the ACA is the enormous amount of effort contributed by American employers toward its successful implementation. Just think about your HR team’s work agenda in the years preceding 2014. While collectively I do not know your opinions on its repeal – I expect few self-insured employers would wish for the ACA to be repealed, in its entirety, now that these health benefits changes have become the norm in your workplace. If you have an opinion to share, please reach out. In the meantime, we will be advocating for thoughtful and transparent policy deliberations, opportunities for public comment, and long lead times for the implementation of any changes. Warm Regards, Louise Y. Probst
BHC Executive Director
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, October 7, 2020
|
|
COVID-19 ushered in previously unimaginable changes in every sector of the American economy and life. During the early months, health care providers found themselves simultaneously on the front lines confronting the virus while responding to steep revenue losses from unprecedented declines in elective services. Locally, many businesses have had their operations and revenue models upended and find their financial futures placed in question. Likewise, many families find themselves in dire financial need and looking for employment in an uncertain economy. Eight months into the pandemic, infections continue to surge and the end is not yet in sight.
The overuse of low value health care services, previously thought to be unstoppable, dropped overnight. Although this created short-term surpluses in employer health spending accounts, several potentially bothersome scenarios remained: worsening employee health due to missed or delayed diagnosis and treatments, steep health care price escalation, and a return to the rampant overuse of medical services with little or no clinical value.
Concerned about the pandemic’s lasting effects on our community, BHC leaders joined together to share learnings and explore options to realize better health for employees and the community and better value from our region’s collective and significant investments in health care coverage. From these conversations, and on behalf of its members and all employers, BHC sent
correspondence
to local health plan and health system leaders urging them to keep health care prices flat, consistent with current economic conditions and for their leadership in shaping a new, higher value health care system for our region.
BHC also invited their suggestions for steps purchasers can take in supporting their transition to higher value.
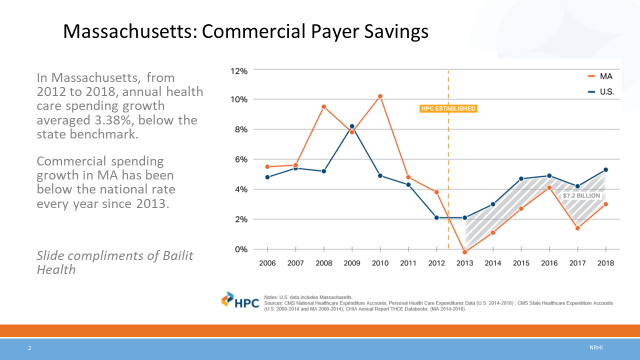
Meanwhile, BHC is actively exploring the successes of other purchasers and leading states on the path to better health and value health care. Some of you with worksites in Massachusetts may already have evidenced the State’s meaningful progress toward more affordable, higher value. Leaving behind a long tradition of being one of the nation’s most expensive health care states, statewide spending targets have enabled it achieve spending well below the national average. In fact, as the Massachusetts Health Policy Commission slide demonstrates, between 2013 – 2018, just the savings from being below the national spending average, freed-up more than $7.2 billion to be spent on other goods and services. We welcome your observations and suggestions.
|
|
Warm Regards,
Louise Y. Probst
BHC Executive Director
|
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, September 2, 2020
Updated: Tuesday, September 1, 2020
|
Flu season is on our doorstep and how we prepare matters. While no one knows what the upcoming flu season will bring, Dr. Jay Butler, the Centers for Disease Control, Deputy Director of Infectious Diseases,
has warned that the flu and COVID-19 could be circulating together as we move into the fall and winter months stating, “If anything, we must over prepare for what we might face later this year.” Preparing means that everyone, 6 months and up gets a flu vaccine, particularly those that are pregnant, over the age of 65 or have a chronic illness.
According to the CDC, the 2019 – 2020 flu season
was mild. Still, there were between 39 million to 56 million cases of the flu, up to 740,000 hospitalizations and between 24,000 to 62,000 deaths. Add COVID-19 infections and this potential “twindemic,” or simultaneous outbreak of these two serious
infections, could overtax regional health care systems and be catastrophic for patients trying to fight off both conditions at once.
Some fear that with COVID-19 center stage the public may forego the annual flu vaccine. Stay at home orders, fewer workers coming into the office and hesitancy to utilize elective
medical services while COVID-19 looms could all deter people from getting their flu vaccine this year. As it is, in a normal year, only about half of the population gets a flu shot.
Employers can help bolster these numbers by helping employees understand that, in the face of the pandemic, the flu shot is an essential part of protecting their and their family’s health and fulfilling their civic duty. Taking definitive action, the
University of California
system recently in the face of the pandemic announced that because of the pandemic, it is requiring
all 230,000 employees and 280,000 students to get the flu vaccine
by November 1.
The potential of vaccines is enormous; it is one way we can each make a difference in our community. To find educational resources to share with your employees and to learn about discounted flu shot pricing available from BHC preferred vendors, please click here.
Warm Regards,
Louise Y. Probst
BHC Executive Director
This post has not been tagged.
Permalink
| Comments (0)
|
|
|
Posted By Louise Probst,
Wednesday, August 5, 2020
Updated: Wednesday, August 5, 2020
|
Last week, President Trump issued Executive Orders intended to restructure the prescription drug market. If they sounded familiar to you, they were. The President directed similar actions from the Rose Garden early in his Administration, only to have them dismissed in the months that followed. The reasons for dismissal included significant implementation challenge, uncertain impact on Medicare drug spending, and questionable enforceability by Executive Order.
Driven by an abundance of evidence that American workers shoulder an unfair and heavier drug spend burden than the workers of other industrialized nations, the President’s action is correctly directed. Even more concerning is the mounting evidence that this gap is widening.
A Painful Pill to Swallow: U.S. vs. International Prescription Drug Prices is rich in detail. Prepared by the Ways and Means Committee staff, the report confirms that the United States’ disproportionately high drug spend is driven more by differences in price than utilization. Drug prices in the U.S. are significantly higher than 11 other nations, being nearly four times higher than average prices. Most notable for plan sponsors: U.S. consumers pay significantly more for drugs than other countries, even when accounting for rebates.
Other nations began taking actions years ago to counter high and escalating drug prices, despite spending dramatically less than the U.S. Ongoing comparisons of drug spending trends demonstrate their success and the widening gap of missed opportunity for U.S. workers. Two common strategies employed are: (1) reference pricing, based on prices set in other nations, and (2) requirements that prices be aligned with evidence of unique clinical value. Both strategies are hallmarks of American values for innovation and competition.
So why have U.S. lawmakers and dominant market players failed to deliver effective solutions? Is it a lack of will or innovative genius? COVID-19 has so clearly revealed the cost of allowing health care spending to crowd out investments in public health and other critical infrastructure. It is time for action.
Warm regards,
Louise Y. Probst
BHC Executive Director
This post has not been tagged.
Permalink
|
|
|
Posted By Louise Probst,
Wednesday, July 1, 2020
Updated: Tuesday, June 30, 2020
|
Employers increasingly see a need to address the emotional fallout of the coronavirus crisis, even as they focus on protecting their employees’ physical health. Improving resilience and emotional well-being is critical during these challenging times, which is why workplace mental health will be the spotlight of the 2020 BHC Summer Forum on July 29.
There is mounting evidence that Americans are experiencing COVID-19 as a serious threat to their mental health. A study by Express Scripts found that the use of prescription drugs to treat anxiety, depression, and insomnia spiked between mid-February and mid-March of this year, with prescriptions for anti-anxiety medications alone rising 34%. Of the prescriptions issued during this period, more than three-quarters were new prescriptions. Just months into the pandemic, more than a third of households contacted by the Census Bureau reported symptoms of clinical anxiety or depression.
It’s clear that the pandemic is exacting a tremendous psychological toll, which can severely impact employee focus and retention. Many Americans worry that they or a loved one will get infected. Juggling work and childcare, fear of job loss, and loneliness are other common sources of stress. Experts say people with pre-existing mental health or substance use disorders are at increased risk.
Workplaces have diligently implemented new routines to prevent the spread of infection, with checklists that include social distancing, temperature checks, and a doubling down on disinfectant. Yet there is a gap in guidelines for navigating the pandemic’s psychological effects.
In fact, the COVID-19 crisis has exposed the cracks in our already fragile mental health system. Unfortunately, the workplace is often the last place where mental health is discussed. According to the National Alliance on Mental Illness (NAMI), roughly 85% of employees' mental health conditions were undiagnosed or untreated before the virus struck. This despite estimates that mental health conditions cost employers more than $100 billion and 217 million lost workdays each year.
Fortunately, there are many resources available for employers who want to step up and effectively support their employees, and the BHC’s 2020 Summer Forum is a great place to start. Join over 300 benefit and wellness leaders to learn about best practices for increasing awareness, decreasing stigma, and creating a culture of health. Featured speakers will include Dr. Charles Zorumski, Head of the Department of Psychiatry at the Washington University School of Medicine, and Mettie Spiess, CEO and Founder of A World Without Suicide. To learn more and to register for the virtual conference, please click here.
Warm regards,
Louise Y. Probst
BHC Executive Director
This post has not been tagged.
Permalink
|
|